|
|

| Journal of Vascular Access 2005; 6: 88 - 91 |
| Tunneled double-lumen silicone hemodialysis catheter placement in three patients with permanent pacemaker wires: A case study |
K.I. Sombolos1, F.N. Christidou1, G.I. Bamichas1, T.C. Anagnostopoulos1, I.I. Rudenko1, L.C. Gionanlis1, T.A. Natse1
1Renal Unit, G.H “G. Papanikolaou”, Thessaloniki - Greece
|
|
 |
 |
Search Medline for articles by:
  K.I. Sombolos K.I. Sombolos
  F.N. Christidou F.N. Christidou
  G.I. Bamichas G.I. Bamichas
  T.C. Anagnostopoulos T.C. Anagnostopoulos
  I.I. Rudenko I.I. Rudenko
  L.C. Gionanlis L.C. Gionanlis
  T.A. Natse T.A. Natse
|
|
 Printable Format (PDF) Printable Format (PDF)
|
|
 |
 |
|
|
|
ABSTRACT
Permanent pacemaker wires have been described as a cause of central vein stenosis. Furthermore, in hemodialysis (HD) patients with transvenous pacemakers, permanent vascular access (VA) created at the ipsilateral arm is not always successful. We report the use of tunneled double-lumen silicone HD catheters, as permanent VA in three HD patients wearing permanent transvenous pacemakers. In one patient, the catheter was inserted
ipsilateral to the pacemaker site. Catheter-related infections were the most significant complications.
Key Words. Hemodialysis, Catheters, Pacemaker
INTRODUCTION
Central vein stenosis has been described as the result of a complication in permanent cardiac pacemaker placement (1). This stenosis is usually indolent and asymptomatic in most patients. However, in patients with end-stage renal disease (ESRD), the creation of an arteriovenous fistula (AVF) or graft, at the extremity ipsilateral to the pacemaker is associated with a high degree of failure. Teruya et al reported that out of 14 hemodialysis (HD) patients with HD access in the extremity ipsilateral to the pacemaker, 10 patients developed symptoms of subclavian venous stenosis such as venous hypertension and arm swelling, while all eventually lost their access (2). To our knowledge, there are no reports regarding an HD patient with a pacemaker wire, having as vascular access (VA), a tunneled double-lu-men permanent HD catheter. In this paper, we report three such cases.
Case reports
Case 1
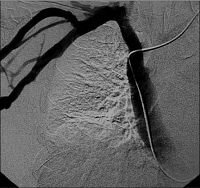
An 82-year-old male with known renal and heart failure was admitted to our dialysis unit with fever, dyspnea, anasarca, bilateral pleural infusions, ascites, hypoproteinemia and oliguria. The serum creatinine (Cr) level was 4.5 mg/dl, blood urea nitrogen (BUN) 81 mg/dl and potassium (K) 5.5 mEq/L. His body weight was 48 kg. The patient was wearing a permanent urinary catheter. A well functioning cardiac pacemaker had been inserted via the left subclavian vein 1 yr previously. Urinary tract infection was diagnosed and antibiotics administered. Furthermore, a temporary double-lumen HD catheter was inserted in the right subclavian vein and HD started. One week later, the patient’s general condition improved. However, the patient suffered from multi-infract dementia and was unable to walk. The family insisted on HD treatment and a permanent, tunneled double-lumen silicone HD catheter was inserted, subcutaneously, in the right subclavian vein. The catheter position was found to be in the inferior vena cava (Fig. 1).
|
|

View larger version |
FIG. 1
Cardiac pacemaker wire and tunneled HD catheter in
case 1. Catheter location,tip in inferior vena cava.
|
|
|
|
Since the catheter was working well (blood flow 300 ml/min, venous pressure 100 mmHg, and urea reduction ratio after 3 hr 60%) it was left in the initial position and the patient continued on HD. His general condition remained stable. Ten months later, the patient developed catheter-re-lated bacteremia due to Staphilococcus aureus and died from septicemia.
Case 2
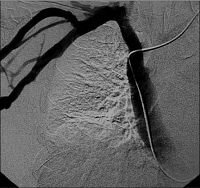
An 83-year-old female was admitted to our dialysis unit with ESRD of unknown origin, dyspnea, leg edema and hyperkalemia. The serum Cr level was 10.2 mg/dl, BUN 122 mg/dl and K 6.9 mEq/L. Herbody weight was 63 kg. A temporary double-lumen HD catheter was inserted in the right jugular vein and HD started. During hospitalization, the patient developed catheter-related bacteremia (Staphilococcus aureus from blood and catheter cultures) that was treated with catheter exchange and antibiotics. The arterial blood pressure ranged from 80-95 mmHg and two attempts of native fistula creation, before pacemaker insertion, were unsuccessful. She also developed a three-bundle branch block with bradycardia and a rate response cardiac pacemaker was inserted via the left subclavian vein. One month later, her general condition had improved and she decided to continue on HD, rejecting continuous ambulatory peritoneal dialysis. A permanent tunneled double-lumen silicone HD catheter was then considered for VA. However, the catheter could not be inserted through the right jugular vein, probably due to vein stenosis at the insertion site. Therefore, a permanent silicone double-lumen HD catheter was inserted, subcutaneously, in the left jugular vein and HD continued. Seven months later, the patient developed a low-grade fever and tunnel infection (Staphilococcus hominis). Antibiotics were administered and the catheter was replaced over a guide-wire. Three months later, the catheter cuff was extruded from the tunnel and the catheter was replaced over a guidewire, while a new subcutaneous tunnel was created. The catheter could not proceed forward easily in the superior vena cava and stopped at a certain point, probably due to fibrin sheath development (Fig. 2).
|
|

View larger version |
FIG. 2
Cardiac pacemaker wire and tunneled HD catheter in
case 2. Catheter location, ipsilateral to pacemaker site |
|
|
|
However, the catheter was working well (blood flow 280 mL/min, venous pressure 120 mmHg, and urea reduction ratio after 4 hr 65%). To date, the patient has completed 21 months of HD treatment using the permanent catheter for VA and her general condition is excellent.
Case 3
A 78-year-old male with chronic renal and heart failure was admitted to our dialysis unit with dyspnea, edema anasarca, bilateral pleural infusions, hypoproteinemia and oliguria. The serum Cr level was 12 mg/dl, BUN 120 mg/dl and K 6.5 mEq/L. His body weight was 101 kg. He had received a cardiac pacemaker via the left subclavian vein, 3 yrs previously, when a complete atrioventricular block was diagnosed. In addition to conservative treatment, a temporary double-lumen HD catheter was inserted in the right jugular vein and HD started. Two weeks later, his general condition improved. As the patient rejected the creation of a native AVF, a permanent double-lumen silicone HD catheter was inserted subcutaneously in the right jugular vein (Fig. 3).
HD treatment continued. Two months later, the patient had a right hip fracture that was treated by surgery. Five months after catheter insertion, the patient developed catheter-related bacteremia due to Staphilococcus epidermidis. Antibiotics were administered and the catheter was changed over a guidewire. The patient was doing well and was in a good overall condition. He had lost 11 kg from his initial body weight and he walked easily using a cane and had regained a certain degree of renal function (residual Cr clearance 7-8 ml/min). After 11 months of HD treatment using the permanent HD catheter for VA, and since his general condition had improved to the maximum, the patient was advised to have a native AVF creation in his right arm. One month later, the catheter was removed and a venography through the fistula confirmed the large veins’ patency (Fig. 4).
|
|
View larger version |
FIG. 4
Venography showing the patency of the large veins after
catheter removal in case 3. |
|
|
|
DISCUSSION
The three clinical cases presented in this paper indicate that tunneled, double-lumen silicone HD catheters can be used for permanent VA in HD patients wearing transvenous cardiac pacemakers. However, specific concerns must be taken into consideration. Pacemaker wires have been implicated as a cause of central vein stenosis and as an occult cause of ipsilateral arteriovenous access failure in HD patients (2, 3). Although less traumatic to large veins, tunneled double-lumen silicone HD catheters can also lead to vein stenosis (4). In our cases, two of the above-mentioned major causes of large vein stenosis coexisted. This can lead to severe large vein stenosis, making it very difficult for the possibility of a successful, upper arm arteriovenous access creation in the future. Moreover, during catheter insertion or during catheter replacement, pacemaker wire dislocation is possible (5). The above were taken into consideration in case 2, when the catheter could not be moved forward easily within the superior vena cava during its replacement. In case 3, however, patency of the large upper body veins was confirmed 11 months after catheter insertion and catheter wire coexistence. Permanent catheter infections and catheter-related bacteremias are frequent complications of permanent double-lumen silicone HD catheters (6). Cardiac pacemaker wires can also be infected and pacemaker endocarditis, although rare, is a well-known complication in patients with transvenous pacemakers (7). Therefore, the use of a double-lumen permanent HD catheter in these patients is another risk for pacemaker infection. One of our patients died from septicemia due to catheter-related bacteremia, while the other two patients each had one episode of catheter-re-ated infection. Although we did not face pacemaker endocarditis in these patients, the risk of its developing is not negligible. From the above it seems that the use of permanent HD catheters in patients with pacemaker wires should be reserved as the last resort as access for chronic HD treatment, although this was not the case in cases 2 and 3, where the patients rejected AVF creation. Catheter dysfunction and thrombosis were not major problems in our patients, and when presented with them they were treated successfully using intraluminal t-PA (three times in case 2 and twice in case 3). In conclusion, our study shows that the use of permanent double-lumen HD catheters is feasible in ESRD patients wearing transvenous cardiac pacemakers.
Address for correspondence:
Kostas Sombolos, MD
Cas. Olgas 82 546 43 Thessaloniki - Greece
sobolos@spark.net.gr
REFERENCES
1. Zuber M, Hubert P, Fricker U, Buser P, Jager K. Assessment
of the subclavian vein in patients with trans-venous
pacemaker leads. Pacing Clin Electrophysiol
1998; 21: 2621-30.
2. Teruya T, Abou-Zamzam A, Limm W. Wong L, Wong
L. Symptomatic subclavian vein stenosis and occlusion
in hemodialysis patients with transvenous pace-makers.
Ann Vasc Surg 2003; 17: 526-9.
3. Chiao-Lin C, Der-Cherng T, Wu-Chang Y, Tung-Po
H. An occult cause of arteriovenous access failure:
central vein stenosis from permanent pacemaker
wire. Am J Nephrol 2001; 21: 406-9.
4. Work J. Chronic catheter placement. Semin Dial
2001; 14: 436-40.
5. Karnatz P, Elsner C, Muller G, Wolter C, Nellessen U.
Permanent pacemaker therapy before and after the
reunification of Germany: 16 years of experience at
an East German regional pacing center. Pacing Clin
Electrophysiol 2000; 23: 991-7.
6. Butterly D, Schwab S. Catheter access for hemodialysis:
an overview. Semin Dial 2001; 14: 411-5.
7. Camus C, Leport C, Raffi F, Michelet C, Cartier F, Vidle
J. Sustained bacteremia in 26 patients with permanent
endocardial pacemaker: assessment of wire
removal. Clin Infect Dis 1993; 17: 46-55.
|
|

 K.I. Sombolos
K.I. Sombolos Printable Format (PDF)
Printable Format (PDF)